

Christenson J, Andrusiek D, Everson-Stewart S, et al.
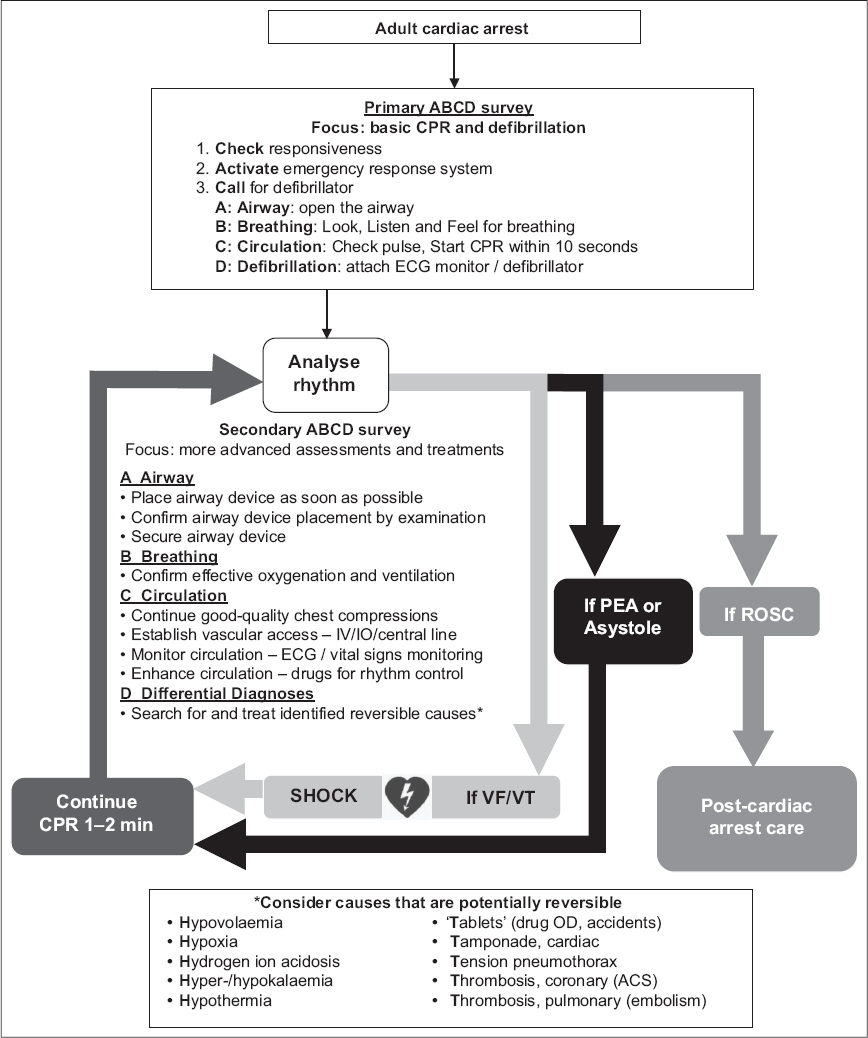
Cardiopulmonary resuscitation quality and patient survival outcome in cardiac arrest: A systematic review and meta-analysis. Westafer is assistant professor of emergency medicine and emergency medicine research fellowship director at the University of Massachusetts Medical School–Baystate and co-host of FOAMcast. Before we debate antiarrhythmics or double sequential defibrillation, let’s get the fundamentals right and stop routinely checking pulses during CPR cycles.ĭr. It is more likely that we believe we have overconfidence in our ability to do simple things well and have difficulty unlearning our fundamental practices. A shift in our language and personnel to tasks that are actionable, creates a simpler and more efficient resuscitation environment that has a better chance of reducing “hands off” time. However, the pulse palpation literature is clear-assessing for a pulse is cognitively taxing. Perhaps some may resist the pivot to rhythm checks, arguing this is only a semantic change. They will hallucinate death (no pulse) four times as frequently-about four out of 10 times.” 11 Despite the authors’ urging, first responders and physicians continue with pulse checks. The authors highlighted pulse checks and summarized the 1996 data, “rescuers will hallucinate a pulse when one is absent about once every 10 arrests. In fact, research continues to focus on “pulse checks.”10A 1999 article in Annals of Emergency Medicine urged clinicians to pay close attention to pivotal shifts in evidence behind common CPR practices as AHA guidelines would certainly change. In both cases, prolonging the pause in chest compressions may have deleterious effects on organ perfusion.Īlthough the AHA guidelines have specified rhythm checks rather than pulse checks for over 10 years, clinicians have been slow to change practice. If a patient is in ventricular fibrillation or ventricular tachycardia, there is no need to feel for a pulse-the treatment is defibrillation. If a patient is in asystole, there is no need to check for a pulse-there will not be one. The goal of the rhythm check is to ascertain whether the patient has an intervenable rhythm-one that is amenable to defibrillation (ventricular fibrillation or ventricular tachycardia) or a potentially perfusing rhythm. Unlike a pulse check, rhythm checks take a few seconds. Rhythm checks allow rescuers to identify rhythms amenable to defibrillation. ACEP member study says pit crew approach with real-time CPR feedback saves livesĮxplore This Issue ACEP Now: Vol 41 – No 08 – August 2022 Rhythm Checks Are “In”ĭuring CPR, advanced cardiac life support (ACLS) guidelines advocate for rhythm checks every two minutes.Interrupting Chest Compressions During CPR Does Not Worsen Survival.Push your understanding of taking care of these patients so you can deliver the best care possibleĬore EM: A Simplified Approach to TachydysrhythmiasĬore EM: Amiodarone, Lidocaine or Placebo in OHCAĮmDocs. Finally, remember that as Emergency Physicians, we are specialists in the resuscitation of cardiac arrests.Consider pre-charging your defibrillator to minimize pauses in CPR and maximize your chance for ROSC.Medications like epinephrine and amiodarone have never been shown to improve good neurologic outcomes in the ACLS recommended doses.In cardiac arrest, the most important interventions are to deliver electricity quickly when it’s indicated and to administer good high-quality compressions with minimal interruptions to maximize your compression fraction.


 0 kommentar(er)
0 kommentar(er)
